When death is near, families often feel two kinds of pressure at the same time. One is emotional: the ache of watching someone you love change, the fear of doing something wrong, the worry that you will miss a moment you can’t get back. The other is practical: medication schedules, phone calls, paperwork, and decisions that seem to arrive faster than your ability to think.
This guide is meant to steady you in both directions. It focuses on comfort first, then logistics, then communication—because those are the three areas that most often determine whether this time feels chaotic or held with care. If your loved one is on hospice or receiving palliative support, your clinical team should always be your first call for symptom changes and safety concerns. This article is educational and not medical or legal advice.
Start With the Goal: Comfort, Not Perfection
Families sometimes carry an invisible expectation that the final days should look a certain way: peaceful, quiet, meaningful, free of conflict, free of fear. In reality, the end of life is often uneven. There may be calm hours and restless hours. There may be hard conversations and tender ones. Your job is not to make this perfect. Your job is to reduce suffering where you can and to keep love present in whatever form is possible.
The National Institute on Aging explains that both hospice and palliative care focus on comfort, care, and quality of life for people with serious illness. When you hold onto that as the guiding principle, decisions become less about “the right choice” and more about alignment: what helps now, what harms now, what supports dignity now.
Comfort When Death Is Near: What Families Can Do (and What to Ask For)
As death approaches, the body often becomes less interested in food, water, conversation, and activity. That can be frightening to witness, especially for caregivers who have been showing love through meals, hydration, and encouragement. If appetite fades, it does not automatically mean someone is “starving.” Often, it reflects the body’s natural slowing. What matters most is comfort: dryness, nausea, anxiety, pain, breathlessness, and whether your loved one can rest.
If hospice is involved, call them early about symptom changes. Hospice teams are trained to adjust plans for pain, shortness of breath, agitation, nausea, and other common end-of-life symptoms. If hospice is not involved but comfort needs are increasing, ask the medical team about palliative support. The goal is not to “tough it out.” The goal is to reduce distress.
Many families find it helpful to focus on a few simple comfort anchors. A calm room. Soft lighting. Fewer competing voices. Gentle repositioning when needed. Basic mouth care (a moist swab, lip balm, small sips if safe and recommended). Warm blankets or cool cloths depending on comfort. Above all, a sense of safety—someone present, someone speaking gently, someone not forcing the body to perform.
If you are unsure what is normal, or you feel afraid that you are missing something urgent, bring your questions to a clinician. This is one place where you should not have to guess.
If Hospice Is Involved: How Support Escalates and Who to Call
Families often assume hospice is one fixed level of help. It is not. Medicare describes four levels of hospice care that adjust to patient and caregiver needs, including routine home care, continuous home care during short crisis periods, general inpatient care when symptoms can’t be managed elsewhere, and inpatient respite care to give caregivers a brief rest. You can read Medicare’s overview here: Hospice Levels of Care. CMS also describes hospice as a comprehensive program with comfort care and symptom management as the focus.
This matters because a common caregiver fear is, “If things get worse tonight, we’ll have no options.” Hospice is designed to give you options. Most hospice programs also provide an after-hours phone line. Ask, explicitly, what happens when you call after hours, how quickly a nurse can come if needed, and what symptoms should trigger an immediate call.
If you’re new to hospice and want a broader overview of what is typically covered under Medicare, start with Medicare Hospice Care and the Medicare Hospice Benefits booklet. Those resources can help families understand why hospice focuses on comfort and what support is meant to be available.
If Hospice Is Not Involved: How Families Get Help Quickly
Sometimes families are in the “in between.” A loved one is seriously ill, but hospice has not started. Or the family is unsure whether hospice is appropriate yet. If you are in that space and death feels near, do not wait for the perfect time to ask for support. Ask the treating clinician directly, “Would hospice be appropriate now?” If the answer is uncertain, ask for a palliative care consult. The National Institute on Aging explains the difference in timing and purpose, which can help families understand why palliative care can begin earlier and hospice typically centers watching, comfort, and family support in the final months.
If coverage questions are part of the hesitation, Medicare’s hospice coverage overview is a good starting point. For some families, simply understanding that hospice is a formal benefit with defined support helps them feel less like they are “asking for special treatment” and more like they are accessing care that exists for exactly this situation.
Family Communication: The Conversations That Prevent Regret
When death is near, communication can either become a source of comfort or a source of friction. Families sometimes fracture because everyone is scared and trying to protect everyone else. One person insists on optimism. Another insists on realism. A third disappears into logistics. None of these roles mean someone loves less. They are coping styles.
If you can do one thing that protects the family, do this: name a point person. Someone who will talk with hospice or the medical team, relay information, and reduce the feeling that everyone has to interpret updates separately. Then name a second role: someone who protects the room. Someone who can gently manage visitors, keep the environment calm, and limit conversations that exhaust the patient.
If your family struggles to talk about wishes, Funeral.com’s guide Talking About End-of-Life Wishes with Family offers language that makes these conversations feel less like a confrontation and more like care. If you need clarity around medical decision tools—who can decide, what documents matter, and how to put wishes in writing—Funeral.com’s Advance Directives and Living Wills is a strong companion read during this time.
If children are involved, consider honest simplicity. Children often sense the truth before adults name it. They do not need graphic detail; they need clarity, reassurance that they will be cared for, and permission to feel whatever they feel. It is also okay to set boundaries: not every child needs to be in the room for every moment, and not every family member needs the same amount of access to the bedside.
Logistics When Death Is Near: Make a “Calm Folder” Before You Need It
Even in a peaceful death, practical tasks appear quickly: documenting a death, contacting a funeral home, obtaining certified copies of the death certificate, handling benefits, and organizing key papers. Families often wish they had gathered these items earlier—not because it changes the outcome, but because it reduces chaos.
One of the most helpful preparation steps is creating a single place for essentials: identification, insurance cards, a medication list, contact information for the hospice team or doctors, and a list of immediate next-of-kin. If the person has expressed preferences about funeral planning, put those notes there too. That might include burial versus cremation, a preferred funeral home, whether they want a service, and who they would want notified.
Funeral.com’s guide Important Papers to Organize Before and After a Death is designed for exactly this moment. It walks through what families scramble for, how to store it, and how to reduce the “where is that paper?” stress that can intensify grief.
What Happens Immediately After Death: The First Calls Depend on the Circumstances
Families often search for what to do in the hours after death, and the answer depends on where and how the death occurs. If your loved one dies at home and the death was expected under hospice care, the hospice team typically guides next steps, including pronouncement and coordination. If a death is unexpected at home, the process may require emergency services and a different set of steps. Funeral.com’s step-by-step resource What to Do When Someone Dies at Home explains expected versus unexpected scenarios in clear language.
If the death occurs in a hospital or facility, staff generally guide next steps, including the required pronouncement and paperwork. Even then, families still face choices about a funeral home, cremation or burial, and how to inform relatives. If you want a steady walkthrough of the overall process, How to Plan a Funeral in 7 Steps is written as a grounding reference for the first wave of decisions.
Death Certificates, Benefits, and Agencies: What Families Commonly Need to Do
After a death, many tasks require certified copies of the death certificate. Funeral.com’s guide Death Certificates: Why You Need Them explains why families often order multiple copies and how replacements typically work.
If you need official guidance on where death records are issued, the CDC explains that to obtain a certified copy you generally contact the vital records office in the state where the death occurred.
Families also worry about Social Security reporting and benefits. The SSA notes that funeral homes generally report the death, but families should contact SSA if a funeral home isn’t involved or doesn’t report it. For a Funeral.com-specific overview of common survivor questions, timing concerns, and what families often need to report, see Social Security and Death. USA.gov also provides a practical overview of agencies families may need to notify and how reporting often flows from the funeral director to SSA and Medicare.
Funeral Decisions Near the End: Create Clarity Without Forcing Details
Some people want every detail planned. Others want only a basic preference documented. Either is valid. The purpose of funeral planning near the end is not to lock your family into a script; it is to leave enough clarity that they can act without guessing.
If you are planning ahead and want a simple structure, Funeral.com’s How to Preplan a Funeral and Preplanning Your Own Funeral or Cremation are designed to help families write down preferences in a way that feels humane, not transactional.
It can also help families to know they have rights when comparing providers and costs. The Federal Trade Commission explains that funeral providers must give a General Price List to anyone who asks in person about funeral goods, services, or prices. That single consumer right can reduce the fear that you’ll be pressured into decisions you don’t understand.
When Cremation Is Chosen: Ashes, Memorialization, and Not Rushing the “Final Plan”
Many families who choose cremation still feel unsure about what happens next. That uncertainty is normal. Some people want to scatter right away. Others want to keep the urn at home for a season. Others want to divide ashes among relatives or choose a keepsake item. You do not have to force a final decision immediately after death.
If your family is considering keeping ashes at home, Funeral.com’s guide Keeping Ashes at Home: How to Do It Safely, Respectfully, and Legally covers practical placement, household comfort levels, and respectful etiquette.
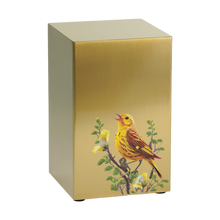
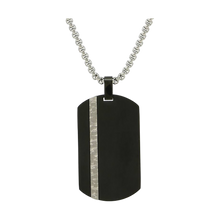
For families who want a central memorial, many begin by browsing cremation urns for ashes to find a style and material that feels right for the home or for cemetery placement. When multiple loved ones want a meaningful portion, keepsake urns can reduce conflict and help each person hold remembrance in their own way. And for those who want something discreet and wearable, cremation jewelry—including cremation necklaces—is designed to carry a small, symbolic amount close to the heart.
A Final Note: You’re Allowed to Need Support
When death is near, it is common to feel both love and exhaustion, tenderness and numbness, clarity and disbelief. None of those emotions disqualify you from being a good caregiver or a good family member. They are part of what the nervous system does when it is under strain.
If you’re reading this in the middle of a hard week, let the priorities be simple. Comfort first. Then the minimum logistics that keep the next days stable. Then communication that prevents conflict and regret. You do not have to carry every task alone, and you do not have to be perfectly composed to show up with dignity. Presence, honesty, and a few steady steps are enough.